Aurora Panic Disorder (APD), characterized by unexpected anxiety attacks, significantly impacts daily life with physical symptoms and fear of recurrence. Effective therapy combines cognitive-behavioral therapy (CBT) to challenge negative thoughts, mindfulness exercises, relaxation techniques, and support groups for holistic management. Early detection through Crisis Intervention Guidance and Mental Health Policy Analysis is crucial, empowering professionals to offer accurate diagnosis and CBT for APD, enhancing quality of life and destigmatizing mental illness, particularly among young adults experiencing anxiety attacks.
Mental illness diagnosis accuracy is a critical aspect of patient care, especially for conditions like Aurora Panic Disorder (APD), which often goes undiagnosed or mismanaged. This article delves into APD’s defining characteristics, its impact on daily life, and the unique challenges it presents in diagnosis. We explore common misconceptions and stigma surrounding mental health, highlighting how these barriers hinder accurate identification. Furthermore, we discuss innovative therapy approaches, including evidence-based treatments for anxiety attacks, integrated care models, the role of technology, and patient education, all geared towards enhancing diagnostic accuracy and improving mental well-being.
- Understanding Aurora Panic Disorder and Its Impact
- – Definition and symptoms of Aurora Panic Disorder
- – Prevalence and affected demographics
Understanding Aurora Panic Disorder and Its Impact

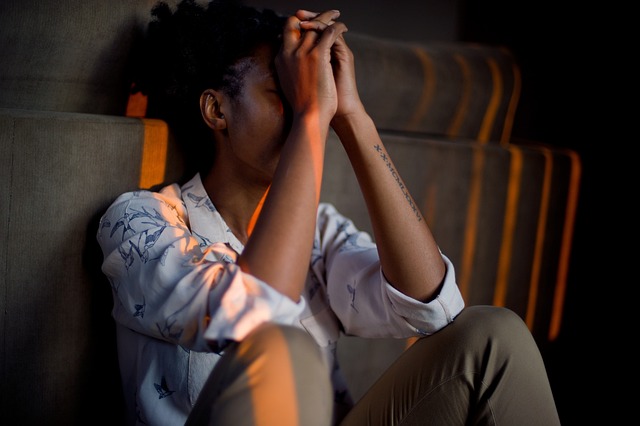
Aurora Panic Disorder (APD) is a complex mental health condition characterized by recurrent and unexpected panic attacks, significantly impacting an individual’s daily life. These sudden episodes of intense fear or discomfort often include physical symptoms like rapid heartbeat, sweating, and shortness of breath, leaving sufferers feeling as if they are in immediate danger. APD can lead to a persistent fear of having future panic attacks, which may result in avoidance behaviors and a significant decline in overall quality of life.
Effective therapy for APD typically involves cognitive-behavioral therapy (CBT), which helps individuals challenge and change negative thought patterns related to their panic attacks. By learning coping strategies and self-care routines, such as mindfulness exercises and relaxation techniques, patients can develop better stress management skills. Additionally, participating in support groups or workshops focused on mental wellness can provide a safe space for sharing experiences and gaining insights from others facing similar challenges, ultimately enhancing the overall effectiveness of therapy.
– Definition and symptoms of Aurora Panic Disorder

Aurora Panic Disorder (APD) is a severe mental health condition characterized by sudden and recurrent episodes of intense fear or anxiety, known as panic attacks. These attacks can occur unexpectedly, causing individuals to experience physical symptoms such as rapid heartbeat, sweating, trembling, shortness of breath, and chest pain. People with APD often live in constant fear of the next attack, which can significantly impact their daily lives and overall mental wellness.
Effective therapy plays a pivotal role in managing APD. Cognitive-behavioral therapy (CBT) is commonly used to help individuals identify and change negative thought patterns contributing to anxiety. Through CBT, patients learn coping strategies to manage panic attacks and reduce the intensity of fear responses. Additionally, stress management workshops organized by mental health organizations can empower individuals with tools to regulate stress levels, a key factor in preventing and controlling anxiety episodes. Community outreach programs focused on raising awareness about APD also contribute to destigmatization, encouraging those affected to seek professional help and support.
– Prevalence and affected demographics

Mental illness, a pervasive global concern, affects millions across diverse demographics. Studies indicate that anxiety disorders, such as Aurora Panic Disorder characterized by recurrent and intense anxiety attacks, are among the most prevalent mental health issues worldwide. This disorder disproportionately impacts young adults, with symptoms often surfacing during adolescence or early adulthood. The impact is significant, leading to decreased quality of life, functional impairment, and increased risk for suicide.
Efforts towards enhancing diagnosis accuracy focus on both clinical practice improvements and policy-level interventions. Crisis Intervention Guidance plays a crucial role in immediate assessment and support, while Mental Health Policy Analysis and Advocacy drive systemic changes. Boosting confidence among mental health professionals is another key strategy to ensure early detection and effective therapy, like cognitive behavioral therapy for Aurora Panic Disorder, which has proven beneficial in managing anxiety attacks and improving overall well-being.
Mental health professionals are continually working to improve diagnosis accuracy, especially for lesser-known conditions like Aurora Panic Disorder. By raising awareness about its unique symptoms and demographic prevalence, we can ensure better access to targeted therapy for those suffering from anxiety attacks associated with this condition. Through ongoing research and education, the field of psychiatry aims to provide more effective support for individuals navigating the challenges of Aurora Panic Disorder.